What is Neulasta®?
Neulasta® is a prescription medicine used to help reduce the chance of infection due to a low white blood cell count, in people with certain types of cancer (non-myeloid), who receive anti-cancer medicines (chemotherapy) that can cause fever and low blood cell count.
To learn more about how Neulasta® works, watch the video here.
Who should receive Neulasta®?
Neulasta® is a prescription medication used to help reduce the chance of infection due to a low white blood cell count, in people with certain types of cancer (non-myeloid), who receive anti-cancer medicines (chemotherapy) that can cause fever and low blood cell count. Talk to your doctor to see if Neulasta® may be appropriate for you.
Who should not take Neulasta®?
Do not take Neulasta® if you have had a serious allergic reaction to Neulasta® (pegfilgrastim) or to NEUPOGEN® (filgrastim). Talk to your doctor to see if Neulasta® may be appropriate for you.
What should I tell my healthcare provider before taking Neulasta®?
Before you receive Neulasta®, tell your healthcare provider if you:
- Have sickle cell trait or sickle cell disease
- Have had severe skin reactions to acrylic adhesives
- Are allergic to latex
- Have problems with your kidneys
- Have any other medical problems
- Are pregnant or plan to become pregnant. It is not known if Neulasta® may harm your unborn baby.
- Are breastfeeding or plan to breastfeed. It is not known if Neulasta® passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Learn more about what to discuss with your doctor with our doctor discussion guide here.
How does strong chemotherapy result in low white blood cell counts?
While chemotherapy is fighting cancer cells, it can also harm normal cells in the body that divide rapidly. Strong chemotherapy described as myelosuppressive (my-eh-lo-suh-press-iv) can lower the number of infection-fighting white blood cells called neutrophils in your body. White blood cells are a key part of your immune system.
Learn more about the role of white blood cells here.
What kind of drug is Neulasta®?
Medications like Neulasta® may be called white blood cell boosters because they help your body produce more infection-fighting white blood cells during strong chemotherapy. These medications are man-made forms of a substance called granulocyte (gran-yoo-loh-site) colony-stimulating factor (G-CSF) that is naturally produced by the body. They stimulate the growth of a type of white blood cell called neutrophils, which are important in the body's fight against infection.
What if I'm prescribed a biosimilar to Neulasta?
A biosimilar is a highly similar version of an approved biologic medicine. Biologics and biosimilars are both made from living cells. Biosimilars must provide the same treatment benefit as the original biologic.
Only Neulasta has an FDA approved on-body injector called Neulasta Onpro.
How does Neulasta® work?
Neulasta® works like a natural protein in your body to promote the growth of new white blood cells. Neulasta® helps protect against the risk of infection and is a prescription medication given approximately 24 hours after you receive chemotherapy treatment to help protect you through that cycle.
To learn more about how Neulasta® works, watch the video here.
What are the study results for Neulasta®?
In a key study of 928 patients with breast cancer who received up to 4 cycles of strong chemotherapy, one group of patients received Neulasta® (the study group), while the other group did not receive Neulasta® (the placebo group). Neulasta® was shown to help protect against the risk of infection with fever (sometimes called febrile neutropenia or neutropenic fever) through strong chemo treatment. The most common side effect experienced with Neulasta® was aching in the bones or muscles.
To see more data, view the information here.
What are the possible serious side effects of Neulasta®?
The possible serious side effects of Neulasta® include:
- Spleen Rupture. Your spleen may become enlarged and can rupture while taking Neulasta®. A ruptured spleen can cause death. Call your doctor right away if you have pain in the left upper stomach area or left shoulder tip area. This pain could mean your spleen is enlarged or ruptured.
- A serious lung problem called Acute Respiratory Distress Syndrome (ARDS). Call your healthcare provider or get emergency medical help right away if you get any of these symptoms of ARDS: fever, shortness of breath, trouble breathing, or a fast rate of breathing.
- Serious Allergic Reactions. Get emergency medical help right away if you get any of these symptoms of a serious allergic reaction with Neulasta®: shortness of breath, wheezing, dizziness, swelling around the mouth or eyes, fast pulse, sweating, and hives.
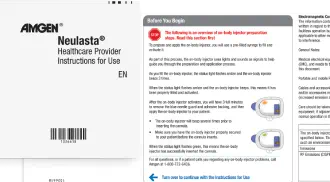
If you have an allergic reaction during the delivery of Neulasta®, remove the on-body injector for Neulasta® by grabbing the edge of the adhesive pad and peeling off the on-body injector. Get emergency medical help right away.
- Sickle Cell Crises. Severe sickle cell crises, and sometimes death, can happen in people with sickle cell trait or disease who receive filgrastim, a medicine similar to Neulasta®.
- Kidney injury (glomerulonephritis). Kidney injury has been seen in patients who received Neulasta®. You should notify your healthcare provider right away if you experience puffiness in your face or ankles, blood in your urine or brown colored urine or you notice you urinate less than usual.
- Increased white blood cell count (leukocytosis). Your doctor will check your blood during treatment with Neulasta®.
- Capillary Leak Syndrome. Neulasta® can cause fluid to leak from blood vessels into your body's tissues. This condition is called "Capillary Leak Syndrome" (CLS). CLS can quickly cause you to have symptoms that may become life-threatening. Get emergency medical help right away if you develop any of the following symptoms:
- Swelling or puffiness and are urinating less often
- Trouble breathing
- Swelling of your stomach-area (abdomen) and feeling of fullness
- Dizziness or feeling faint
- A general feeling of tiredness
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Neulasta®. For more information, ask your doctor or pharmacist.
What are the most common side effects of Neulasta®?
The most common side effect of Neulasta® is pain in the bones and in your arms and legs. Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of Neulasta®. For more information, ask your doctor or pharmacist.
For additional Important Safety Information, see below.
Do I need to be aware of any drug interactions with Neulasta®?
No formal drug interaction studies have been conducted. When discussing your treatment options, tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
What are the ingredients in Neulasta®?
The active ingredient in Neulasta® is pegfilgrastim. Inactive ingredients in Neulasta® include acetate, sorbitol, polysorbate 20, and sodium in water for injection.
Are there any co-pay and reimbursement resources available for patients prescribed Neulasta®?
Amgen Assist 360™ can help patients with insurance benefit verification and put them in touch with programs that may help them afford their prescribed medication, such as Neulasta FIRST STEP® or other independent nonprofit organizations.
Resources include referrals to independent nonprofit patient assistance programs. Eligibility for resources provided by independent nonprofit patient assistance programs is based on the nonprofits’ criteria. Amgen has no control over these programs and provides referrals as a courtesy only. Call 1-844-MYNEULASTA (1-844-696-3852) to learn more visit the Paying For Neulasta® Onpro® page here.
How will I receive Neulasta®?
Neulasta® is given as an injection under the skin at least 24 hours after you receive chemotherapy treatment to provide protection through that cycle. There are two ways in which you may receive your Neulasta®— either Neulasta® by manual injection or Neulasta® Onpro®. Your healthcare provider will choose with you which one is most appropriate.
Do I have to return to the doctor’s office the day after chemotherapy to get my Neulasta® injection?
Neulasta® is given as an injection under the skin at least 24 hours after you receive chemotherapy treatment to provide protection through that cycle. There are two ways in which you may receive your Neulasta®— either Neulasta® by manual injection or Neulasta® Onpro®. Your healthcare provider will choose with you which one is most appropriate.
If you and your doctor decide to use Neulasta® Onpro®, you may not have to return to the doctor the day after chemotherapy just for a Neulasta® injection.
If, for any reason, you believe you did not receive your full dose of Neulasta® or that your on-body injector is not working correctly, immediately contact your healthcare provider.
To learn more about the benefits of staying home with Onpro®, click here.
*If, for any reason, you believe you did not receive your full dose of Neulasta® or that your on-body injector is not working correctly, immediately contact your healthcare provider, as an incomplete dose could increase infection risk.
Who should I contact if I have additional questions about Neulasta®?
Talk to your doctor for more information on Neulasta®, or call the Neulasta® Support Line toll-free 1-844-MYNEULASTA (1-844-696-3852).